»Innovative technology for your patient’s outcome«
> Device application
Electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) is a modern and sophisticated treatment for specific mental illnesses. In the course of the treatment, the patient is given a short anaesthesia, the muscles are relaxed and the body is supplied with sufficient oxygen, before a short stimulation of the brain is applied. The brain reacts to this with strong activation, after which various, mainly chemical, reactions of the nervous tissue develop, which ultimately lead to recovery. To that extent, ECT resembles to a defibrillation treatment of the heart, which corrects severe cardiac arrhythmias, but ECT requires much lower amounts of electricity. In the following frequently asked questions about ECT are answered.
Electroconvulsive therapy (ECT) at a glance
- Indication
- Effect
- Side effects
- Counter indication
- Course of treatment
- Patient information
- Course of therapy
- Affective psychoses:
- Depression, especially treatment resistant (Largest patient population >80% of all ECT patients)
- Mania, mixed states
- Schizophrenia, especially with acute symptoms (positive symptoms)
- Rarely in: puerperal psychoses, during pregnancy (avoidance of medication) and children, pernicious catatonia, malignant neuroleptic syndrome, severe psychotic compulsive symptoms, Parkinson’s disease, status epilepticus
- Clinical:
- Primarily in the case of life-threatening exacerbations, also suicidality, if indicated also at the express request of the patient,
- Secondarily in the case of pharmacoresistance
- Tied to a generalized seizure
- Not the seizure itself, but the induced neurochemical and neurophysiological processes
- Compensation of disturbed neurotransmitter functions (serotonin, dopamine)
- Recovery of disturbed brain functions (frontal cortex)
- Likely also positively neurotrophic
- One of the safest therapy methods (when considering the treated risk patient population)
- Mortality < 2/100 000 (mainly due to cardiovascular complications)
- Memory impairment (anterograde, persisting only for hours, retrograde rarely in individual cases persisting)
- The ability to learn is retained and usually improves during the course of the treatment
- Very rarely persistent loss of individual content (but also interferences with underlying disease)
- Volatie neurophysiological failures (aphasia, apraxia, agnosia); short and mostly incomplete paresis
- Postictal confusion and slow reorientation, rarely prolonged seizure or delirium
- Postictal cardiac arrhythmia, hypertension
- Headache, nausea, vomiting (due to the anaesthesia), sore muscles (due to the relaxants)
- No absolute counter indication
- Cerebral infarcations <3 months
- Intracerebral mass with a tendency to edema formation (e.g. metastases)
- Relative counter indication: Unstable vascular malformation (angioma, aneurysm), pheochromocytoma
- Retinal detachment, acute glaucoma
- Severe cardiovascular disease (risk of anaesthesia >3 ASA)
- Congestive heart failure
- Heart attack <3 months
- Dangerous cardiac arrhythmias (cardiologist if necessary)
- Disrupted hypertension
- Before ECT
- Thorough psychiatric examination (anamnesis and findings, see counter indications)
- General physical and neurological examination, dental status
- Laboratory (Blood Analysis and serum, urine), ECG
- Depending on the situation, not routine, chest X-Ray, EEG, CCT/MRI
- Patient information (see below) see below and consent (ECT and anaesthesia)
- To ECT (only in appropriate spatialities with possible emergency treatment)
- 8 hours fasting
- Medication continue: e.g. Antihypertensives, bronchodilators (except theophylline: proconvulsive!), acid blockers, steroids, antiarrhythmics, cave b-receptor blockers (asystole, possibly atropine); Only give after treatment: e.g. Antidiabetics, diuretics, cholinesterase inhibitors (glaucoma); Discontinue if possible: e.g. previous psychotropic drugs, lithium (cognitive side effects), or omit > 24 h, level < 0.4 mmol / l, anticonvulsants, benzodiazepines (sedation preferably with neuroleptics)
- Treatment
- Preparation, removal of jewelry, dentures, access, cleaning and application of stimulation- (UL, BT, BF, see above) and monitoring electrodes
- Preoxygenation, induction of anesthesia (methohexital, thiopental, etomidate, propofol), relaxation (succinylcholine)
- Stimulation, if necessary, titration, UL high stimulus dosage, BL lower
- After ECT
- Awakening phase up to protective reflexes, if necessary, keep the airways clear (relaxation)
- Monitoring for about 2 hours, then breakfast and participation in therapies
- Investigation (side effects, effectiveness)
- Clearly defined and standardized, while being appropriate and individual
- General: Indication, side effects, especially memory disorders (see Side effects)
- Individual: Why ECT, alternatives, risks/benefits, possible revocation
- Start with 2-3 treatments per week, mostly UL (non-dominant hemisphere-, right RUL if right-handed, left LUL if left-handed)
- In the case of severe illness, start of BL (BT, BF) if necessary
- Treatment cycle 6-12 treatments, less or more depending on the diagnosis
- If rapid relapse after discontinuation, maintenance ECT (EEKT), about 1st month 4/month, 2nd-3rd Month 2/month, then 4th-6th Months 1/month (very variable according to course)
- If there is no effect:
- Switch to BT after 4-6 unsuccessful UL treatments
- Check diagnosis
- Concomitant diseases (addiction, internal medicine?, concomitant medication? (especially benzodiazepines)
- Possibly pausing, second series (BT)
- Augmentation (antidepressants, neuroleptics)
Electroconvulsive therapy (ECT) Questions and Answers
Electroconvulsive therapy (ECT) Downloads
Download PDF brochure ECT in 24 questions
The DGPPN brochure can be downloaded here to find out more about the topic.
Download PDF Thymatron ECT in german
Here you can download our brochure for the Thymatron, our ECT device.
Download PDF Thymatron EKT english
Here you can download our brochure for the Thymatron, our ECT device.
Download PDF Thymatron ECT in russian
Here you can download our brochure for the Thymatron, our ECT device.
Download PDF Thymatron ECT in italian
Here you can download our brochure for the Thymatron, our ECT device.
Download PDF Thymatron ECT in swedish
Here you can download our brochure for the Thymatron, our ECT device.
Download PDF DGPPN statement on ECT
Here you can download the statement of the DGPPN to learn more about the topic.
How to use our ECT devices
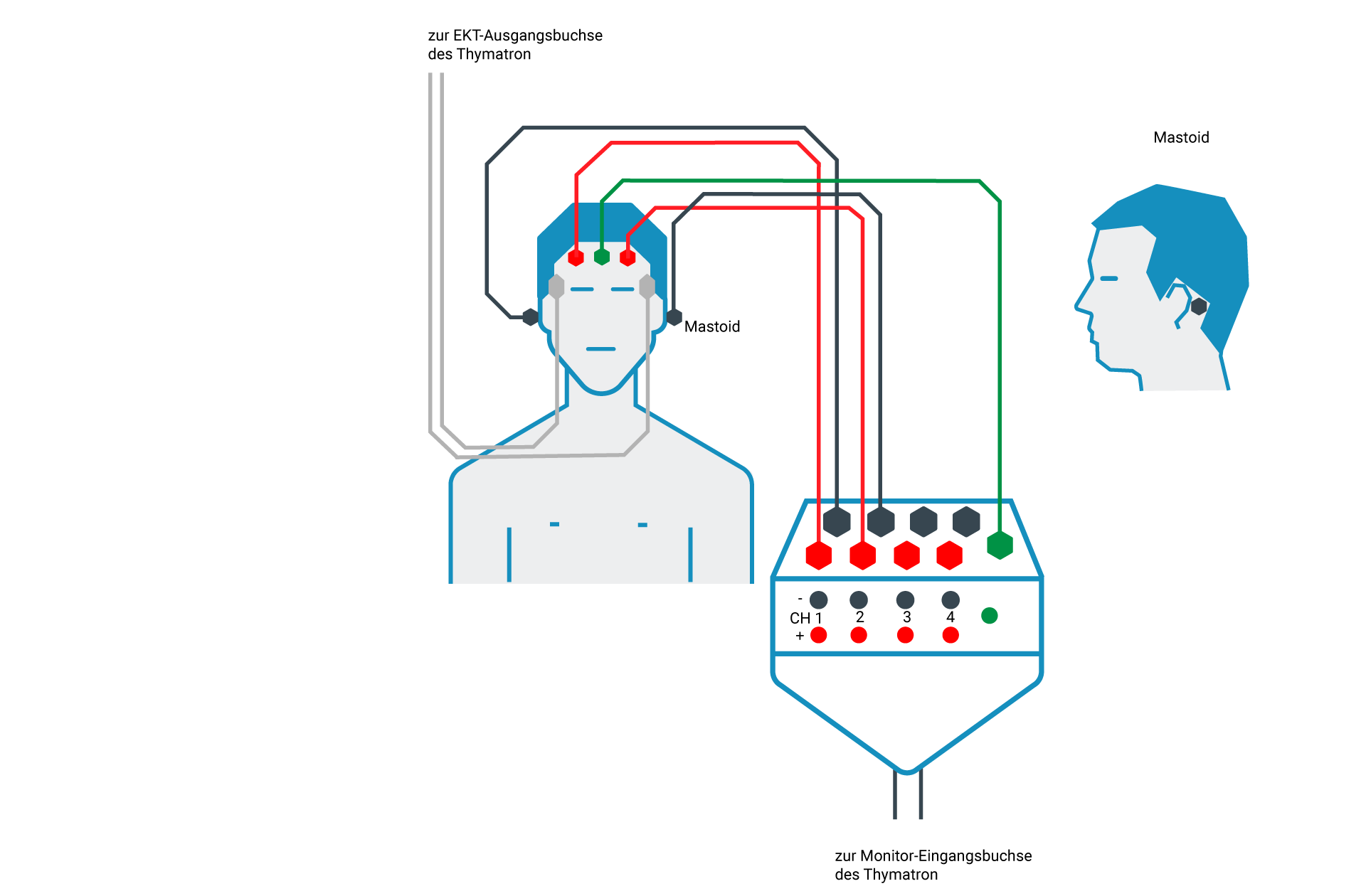
Connection Scheme 1
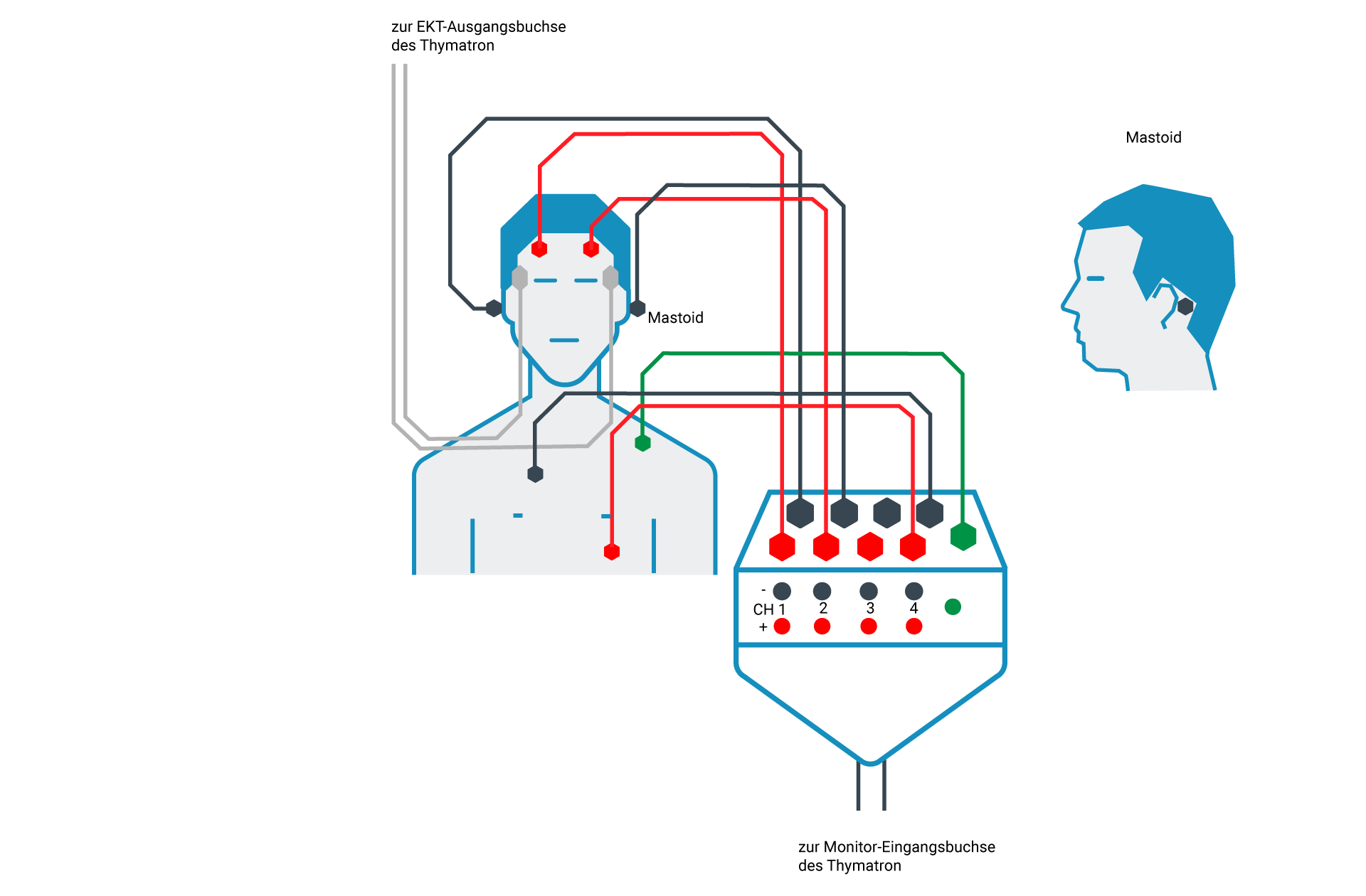
Connection Scheme 2
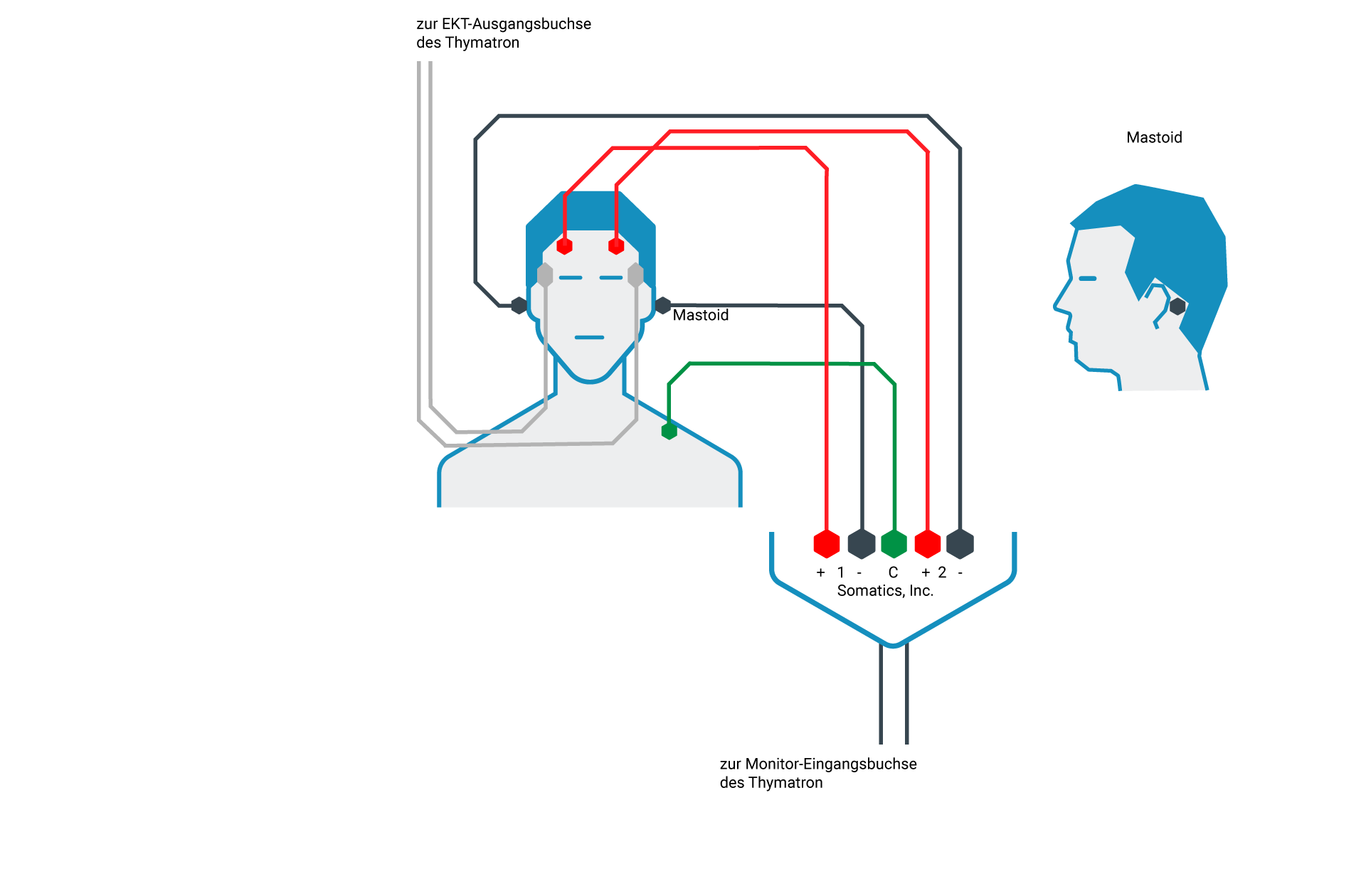
Connection Scheme 3
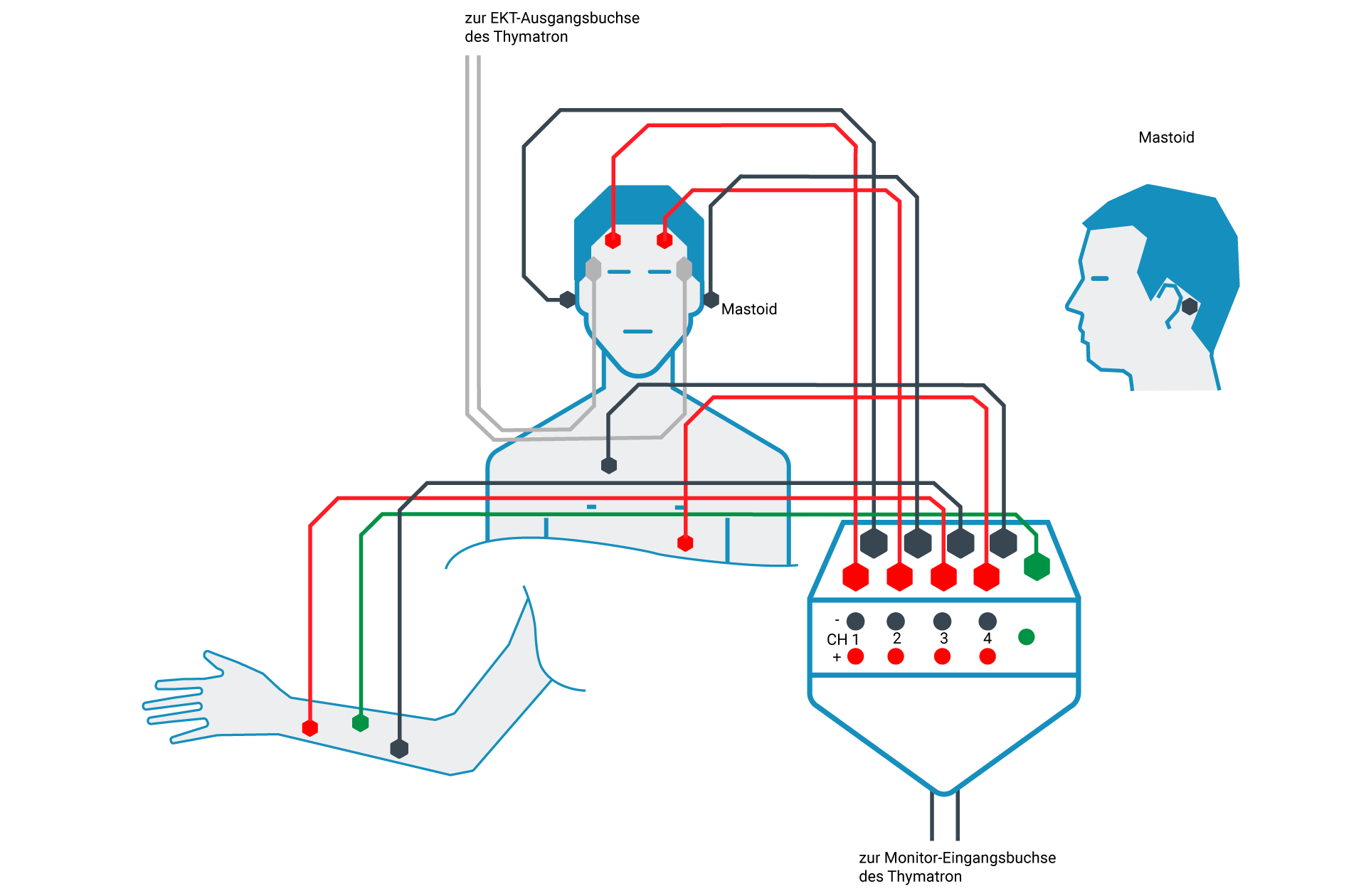
Connection Scheme 4
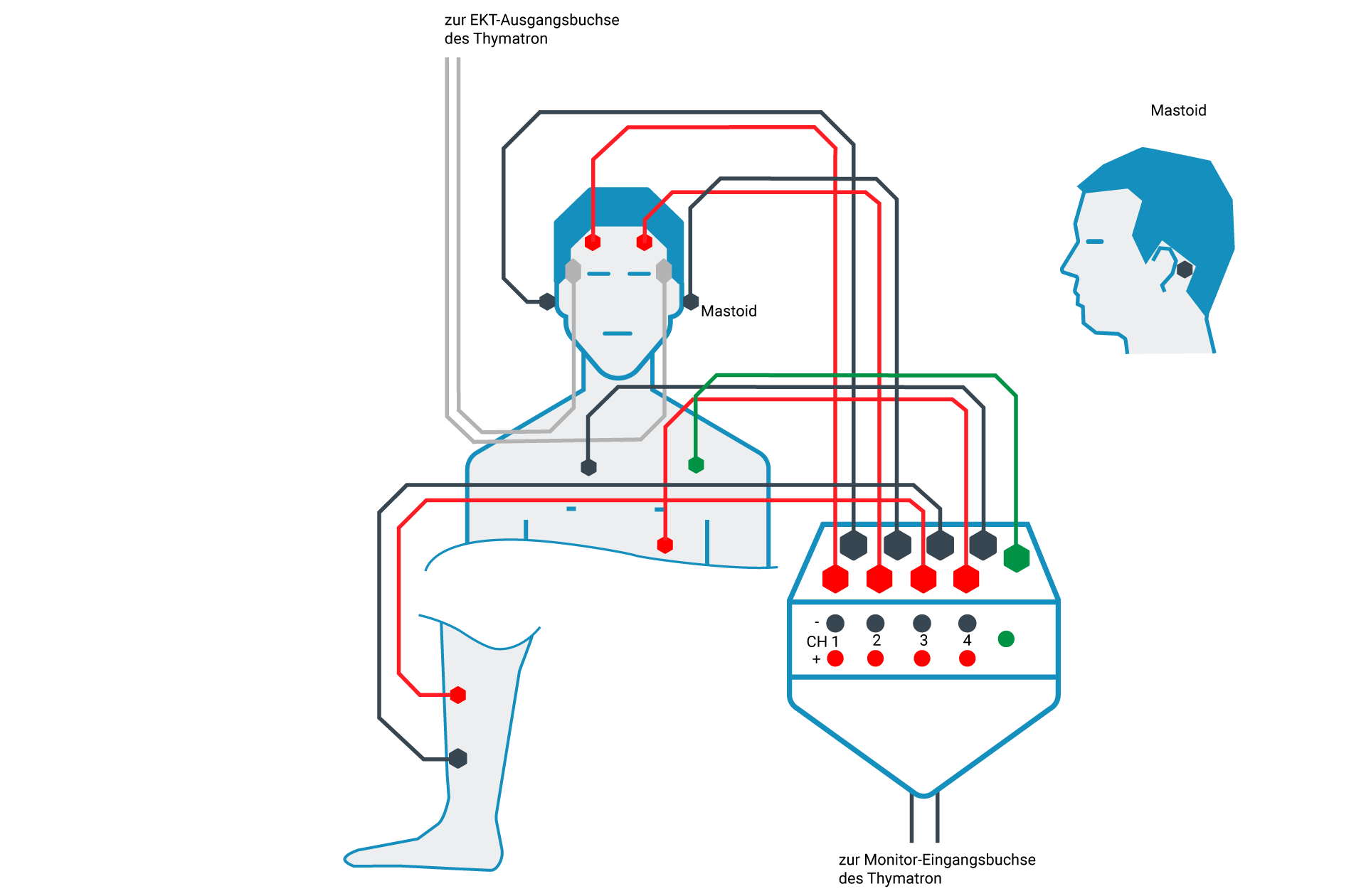
Connection Scheme 5


